HISTORY:
A 50+ year old morbidly obese African American female presents with a 6 month history of an isolated growing, verrucous, pruritic, weeping mass on the left shin that has recently developed a foul odor. She has tried treating at home with alcohol, shea butter, Vaseline and peroxide without improvement. She has daily pitting edema of the lower legs, but has never been diagnosed with lymphedema. Her lower leg skin has become hypertrophic, scaly and hyperpigmented over the course of many years. Her medical history includes hypertension, arthritis, eczema and seasonal allergies.
Is the lesion of concern a squamous cell skin cancer within Elephantiasis Nostras Verrucosa or an ulcerated nodule secondary to ENV?
DIAGNOSIS & CASE SUMMARY:
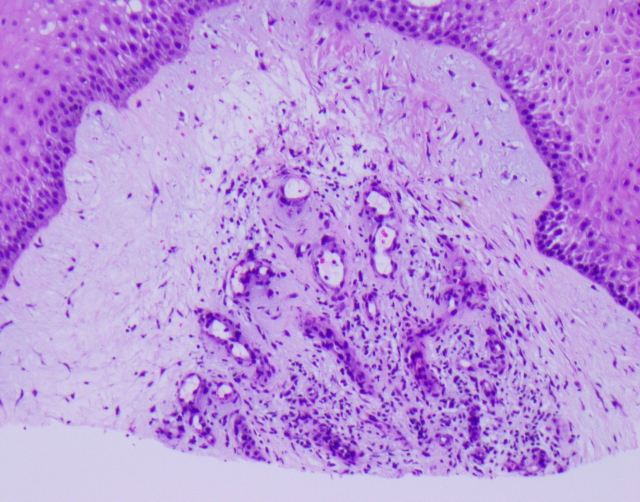
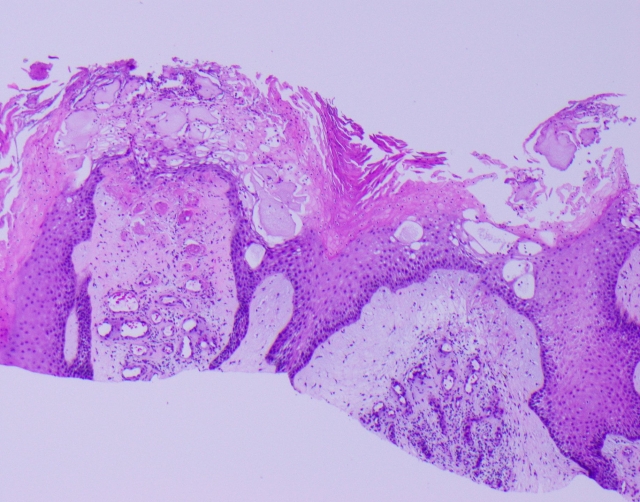
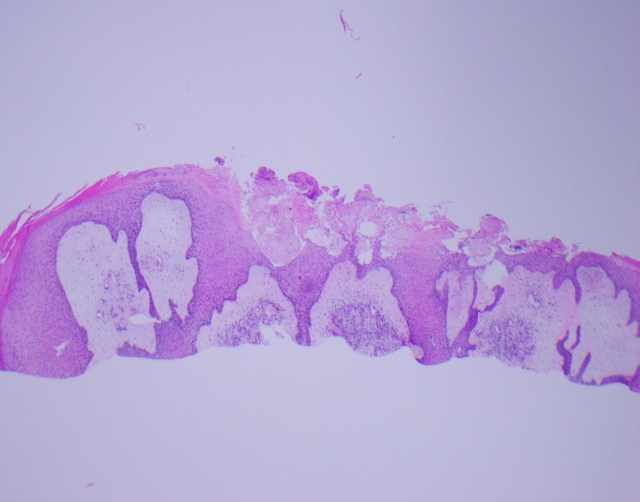
The biopsy shows ulcerated skin with acanthosis, focal verruca keratosis and underlying marked dermal edema with angioplasia, consistent with lymphedema verrucosa nostra (elephantiasis nostras verrucosa). The ulcerated acanthotic mass is secondary to ENV.
SUMMARY:
Elephantiasis Nostras Verrucosa is a complication of chronic lymphedema, most commonly of the lower legs and feet. Over time the chronic lymphedema causes fibrosis and induration, leaving the skin with a cobblestone appearance that is prone to secondary bacterial and fungal colonization. A foul odor is typically associated with these secondary infections. A mainstay of treatment is routine leg wraps or compression socks and a variety of topical keratolytic agents. Some patients may also require topical antimicrobial washes, topical antibiotics, or antifungals if secondary infection is suspected. It is imperative the patient understand the chronic nature of the condition and the long term implications of proper treatment. Many patients with ENV will benefit from the help of physical therapists trained in lymphatic massage and to ensure leg wraps are applied properly and at appropriate intervals to avoid infection or tourniquet-effect from improper wrapping. When the condition is controlled, often patients can graduate to self-applied compression socks for daily wear.
FOLLOW-UP:
This patient was instructed to apply daily 15mmHg below the knee compression socks and wash lower legs daily with CLn Body Wash (sodium hypochlorite wash). Prescriptions were provided for triamcinolone 0.1% ointment BID to the affected area on left lower leg until pruritus is resolved and mupirocin 2% ointment TID to affected areas until follow up. OTC CeraVe SA applied to all other areas of the lower legs daily. Patient was seen for a follow up visit 4 weeks later and was greatly improved with the original mass of concern largely resolved. Following our second visit, a consultation with a local physical therapist who specializes in lymphedema was arranged and she has been seeing patient ever since with no further ulcerations.