HISTORY:
A 60+ year-old male presents with a complaint of widespread skin discoloration. On physical exam, the patient has hypopigmented plaques and patches distributed on his chest and back. He states this started over a year ago in 2020 while he was working as a janitor and denies any known chemical exposure.
Two separate punch biopsies were performed of clinically dimorphic areas.
Which differential diagnoses should be considered?
Click to view enlarged photo.
ANSWER
Eczematous Dermatitis, Vitiligo, and Cutaneous T-Cell Lymphoma
PATHOLOGY
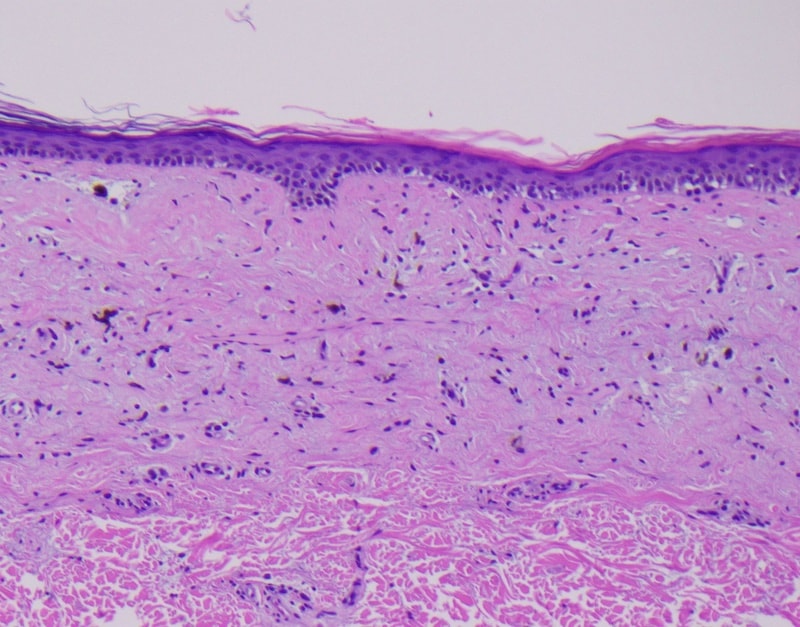
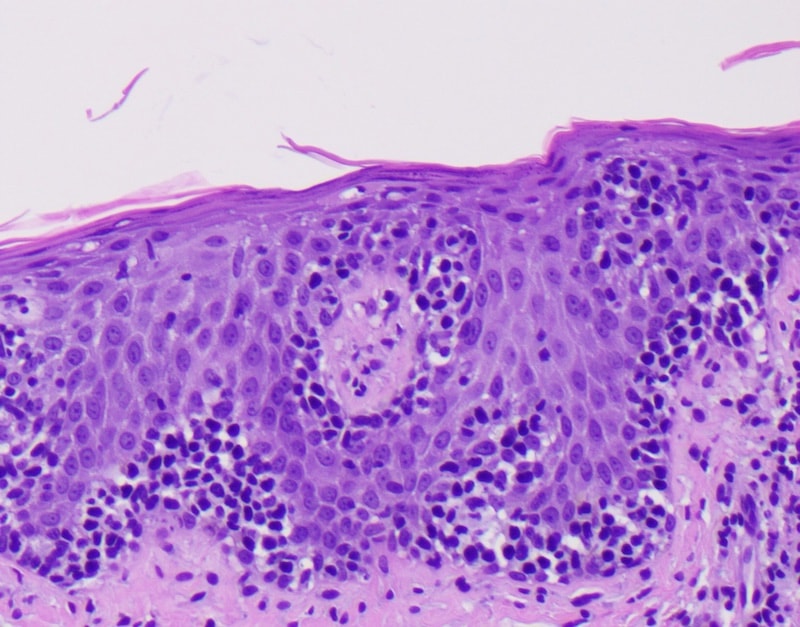
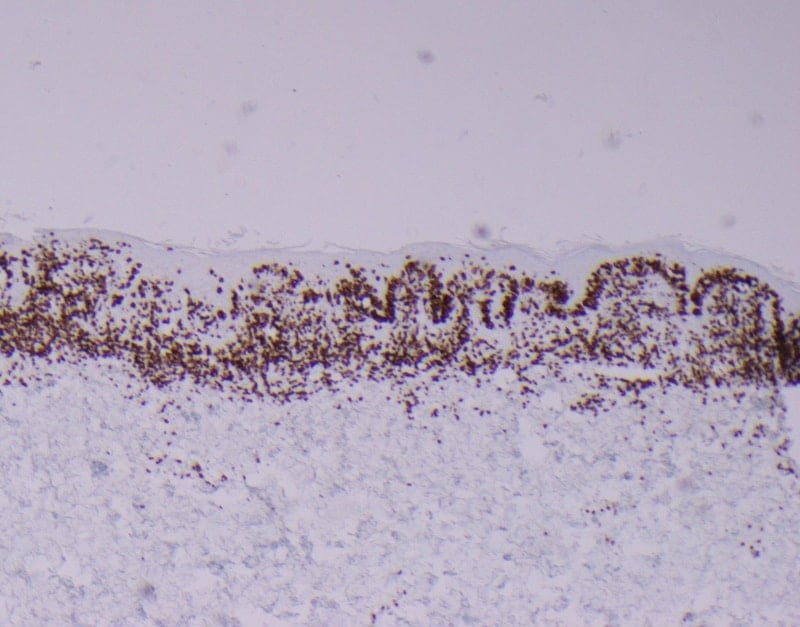
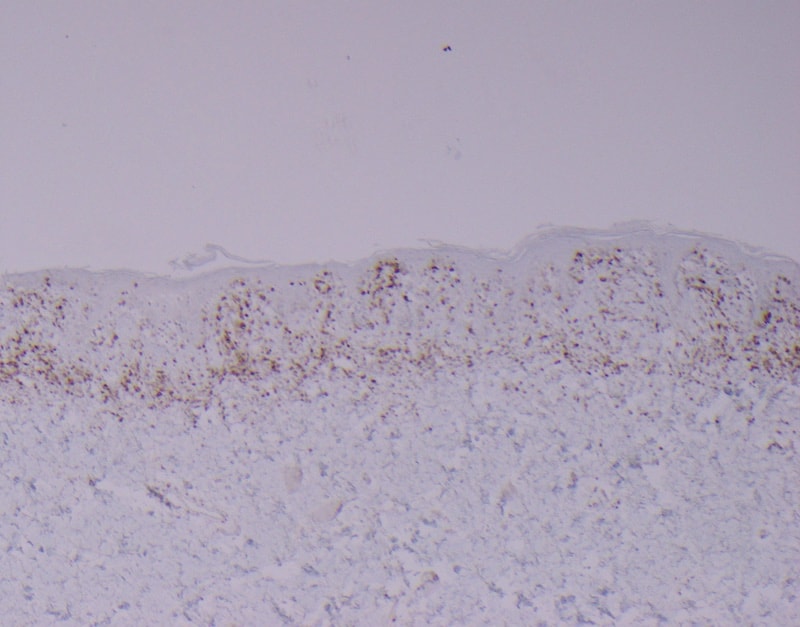
The histology shows two separate histologic phenotypes. The first sample shows an atrophic epidermis with sparse patchy lichenoid inflammation, dermal fibrosis, and pigment drop out. Only rare atypical lymphocytes are identified on the dermal-epidermal junction. The second biopsy shows an acanthotic epidermis with a dense lichenoid infiltrate of hyperchromatic and enlarged lymphocytes. The lymphocytes are distributed in bilayer fashion on the dermal-epidermal junction. Scattered collections of the atypical cells are seen in the epidermis (Pautrier’s microabscess formation). The atypical cells are CD3+ T-cells and demonstrate co-expression for both CD4 and CD8. There is loss of CD7 T-cell marker expression. T-cell gene rearrangement studies performed on the paraffin block are also positive for a clonal TCR gene rearrangement.
DIAGNOSIS & CASE SUMMARY:
Hypopigmented mycosis fungoides (HMF) is characterized by light-colored to achromic lesions, mostly in patches or thin plaques. Nonetheless, tumors have been reported in rare patients. Currently, the most accepted hypothesis surrounding the hypopigmentation and achromia is damaged and reduced numbers of melanocytes in addition to abnormal melanogenesis. HMF lesions are commonly found in non-sun-exposed areas, predominantly on the extremities, buttocks, and trunk in a bathing suit pattern. There are a few documented cases of HMF with facial involvement. The number, size, and shape of lesions are variable, with some case reports.1
HMF tends to be more common in patients with darker skin and in a younger age range than standard mycosis fungoides. The atypical T-cells are more likely to express a CD8+ phenotype than those seen in classic CD4+ expression in non-hypopigmented variants. Atypical T-cells with predominantly CD8+ and CD4- phenotypes have been associated with a better prognosis. Our case, however, appears to express both CD8 and CD4 in the atypical cells. This, combined with the older age of onset, may indicate a more aggressive behavior than typically seen in younger patients with CD8+ CD4- disease.
FOLLOW-UP:
The patient was evaluated and diagnosed, and coordinated care with appropriate imaging and staging with a CTCL clinic was pursued. Staging and treatment results are pending, to be coordinated across multiple specialties.
By: Dr. Luciann Hruza, MD; Dr. Kelli Hutchens, MD; and Dr. Betsy Wernli, MD
References:
- Martínez Villarreal A, Gantchev J, Lagacé F, et al. Hypopigmented Mycosis Fungoides: Loss of Pigmentation Reflects Antitumor Immune Response in Young Patients. Cancers (Basel). 2020;12(8):2007. Published 2020 Jul 22. doi:10.3390/cancers12082007